Category: Blog
Corneal Lipidosis
What is corneal Lipidosis?
Corneal lipidosis is an accumulation of fatty substances (usually cholesterol) within the layers of the cornea.
What causes corneal lipidosis?
There are three main causes of corneal lipidosis: corneal dystrophy, corneal degeneration, and elevated blood cholesterol levels.
Corneal dystrophy is an inherited, or genetic condition and is most commonly seen in dogs. This condition is rarely seen in cats. It is usually present in both eyes. It is not painful and has a minimal effect on vision. Some commonly affected breeds include Beagles, Cavalier King Charles Spaniels, Siberian Huskies, Alaskan Malamutes, Samoyeds, American Cocker Spaniels, Labrador Retrievers, and Collies.
Corneal degeneration occurs secondary to inflammation in the eye and is usually associated with other eye diseases, such as anterior uveitis (inflammation of the iris, choroid, and ciliary body), keratitis (inflammation of the cornea), or scleritis (inflammation of the sclera or white of the eye) Sometimes lipid accumulation is associated with trauma, such as after corneal ulceration that healed with lipid deposits. This is seen more frequently in dogs than cats.
Lastly, elevated cholesterol levels (hyperlipidemia) can cause corneal lipidosis. This may be due to underlying causes such as Cushing’s disease, long-term steroid use, diabetes, or hypothyroidism.
What are the clinical signs of corneal lipidosis?
Lipid deposits in the cornea appear as well-defined areas of sparkly, shiny, or crystalline material. When lipidosis is due to corneal degeneration, other clinical signs may include inflammatory indicators such as eye redness or cloudiness in the eye.

How is corneal lipidosis diagnosed?
Diagnosis is based on a thorough eye examination, including fluorescein dye application, and Schirmer tear test; blood tests, age, breed, and your pet’s history. If your veterinarian suspects hyperlipidemia, then fasting cholesterol, triglyceride, and blood glucose level tests will be recommended.
How is corneal lipidosis treated?

Treatment for corneal lipidosis depends on the cause.
Corneal dystrophy does not require treatment. Your veterinarian will monitor your pet’s eyes periodically to watch for the development of corneal ulcerations.
Corneal degeneration requires treating the primary inflammatory condition in the eye which may include antibiotic or anti-inflammatory eye drops. Your veterinarian may also prescribe pain medication or artificial tear ointment to provide lubrication to the eye and comfort if the corneal surface is irregular.
Lastly, any condition that is causing an elevated cholesterol level must be treated directly in order to reduce the blood cholesterol levels. Dietary management, along with supplementation with additives to reduce cholesterol (flaxseed oil, oat bran, and niacin) can also be helpful in reducing the cholesterol levels.
“If vision is affected or if corneal ulceration occurs multiple times, referral to a veterinary ophthalmologist is recommended.”
If vision is affected or if corneal ulceration occurs multiple times, referral to a veterinary ophthalmologist is recommended.
What is the prognosis of corneal lipidosis?
Corneal dystrophy may resolve on its own and typically does not progress. It usually does not interfere with vision.
The prognosis for corneal degeneration depends on the underlying eye disease. It may progress with chronic inflammation and vision may be affected with advanced disease. Typically, corneal lipidosis does not progress after trauma.
If an underlying disease condition (Cushing’s disease, diabetes, or hypothyroidism) is identified and managed, the prognosis is good. Your veterinarian may recommend periodic blood tests to monitor cholesterol and triglyceride levels.
Contributors: Rania Gollakner, BS, DVM
© Copyright 2019 LifeLearn Inc. Used and/or modified with permission under license.
Smoke Inhalation in Dogs
What is smoke inhalation?
Smoke inhalation injuries can occur with exposure to smoke in large or small quantities. Fires produce a variety of damaging substances, each of which can affect a pet’s airways, lungs, and overall well-being.
Factors that play a role in smoke inhalation include:
• Carbon monoxide. Carbon monoxide is a colorless, odorless gas that is produced in fires. When carbon monoxide is inhaled and enters the bloodstream, it interferes with the body’s ability to deliver oxygen to organs and tissues.
• Hydrogen cyanide. This substance is released when plastic and other synthetic materials burn. Like carbon monoxide, hydrogen cyanide interferes with the body’s usage of oxygen.
• Chemical irritants. Smoke contains a number of chemical irritants. These irritants can trigger airway inflammation and constriction, as well as other lung damage. The irritants found in smoke may vary, depending on the substances that are being burned.
• Thermal injury. The heat contained within smoke can lead to burns within the airways and lungs, triggering severe swelling and inflammation.
What are the signs of smoke inhalation?
Signs of smoke inhalation vary, depending on how much smoke was inhaled, how long the dog remained in smoky conditions, what chemicals were present in the smoke, etc. A pet exposed to small amounts of smoke for a brief period of time will have very different clinical signs than a dog confined in an extremely smoky room for a prolonged period of time.
“The most common sighs of smoke inhailation are respiratory signs.”
The heat and irritants contained within smoke can also cause significant damage to the eyes. Dogs may squint due to pain, the third eyelid may remain up over the eye, and you may also notice inflammation and redness of the eyes (conjunctivitis). Burns may be seen around the face and muzzle. These burns may blister, or may appear as reddened, inflamed areas. If the nostrils are burned, you may notice nasal discharge or visible blisters within the nostrils. If the brain is deprived of oxygen due to smoke inhalation, pets may show neurologic signs. Neurologic signs are common with carbon monoxide inhalation. Signs include weakness, ataxia (impaired coordination, or walking as if drunk), seizures, and/or coma. Dogs may drool excessively or vomit. Dogs with carbon monoxide inhalation also tend to develop cherry red discoloration of the gums.
What tests will my veterinarian perform on my pet?

Your veterinarian will probably begin with pulse oximetry, bloodwork, and radiographs (X-rays) of the chest.
A pulse oximeter is a device that is used to assess your dog’s blood oxygenation. This helps to determine how efficiently your dog’s lungs are working and how effectively your dog is delivering oxygen to his organs and tissues. Pulse oximetry may be ineffective however, in cases of carbon monoxide exposure.
Bloodwork abnormalities can help your veterinarian determine the severity your pet’s lung injuries. Bloodwork findings can guide treatment decisions for your pet, while also providing information to better predict your pet’s prognosis.
Radiographs (X-rays) allow your veterinarian to determine the extent of lung damage that has occurred. In most cases, these changes are visible immediately. In many cases however, these changes will continue to progress over 48-72 hours after the initial injury. Radiographs are often repeated several times during the first 72 hours of treatment, providing a way for your veterinarian to monitor your pet’s lung damage and adjust treatment as needed.
An electrocardiogram (ECG) may also be performed, to assess your pet’s heart rate and rhythm. Oxygen deprivation can lead to heart damage, which may be detected using the ECG.
The heat associated with smoke inhalation and fires often results in ulceration of the eyes. Therefore, your veterinarian may perform a corneal stain or other ophthalmologist tests to assess your dog’s eyes and rule out injuries such as corneal ulceration.
How is smoke inhalation treated?
The treatment of smoke inhalation depends upon the severity of your dog’s signs. In most cases, the injuries seen with smoke inhalation progress over 48-72 hours; therefore, you can expect that your dog will probably be hospitalized and monitored for at least 72 hours.
“The treatment of smoke inhalation depends upon the severity of your dog’s signs.”
In the early stages, most cases of smoke inhalation are treated with oxygen therapy. Oxygen clears carbon monoxide from the bloodstream, improving oxygen delivery to the body’s tissues. Your dog may be placed in an oxygen cage, where concentrated oxygen can be delivered in a way that is non-stressful. If your veterinarian does not have an oxygen cage, they may administer oxygen via facemask or ‘flow-by’ oxygen (holding an oxygen tube near your dog’s face). If your dog has extreme upper airway swelling that prevents breathing, your veterinarian may need to place a tracheotomy tube (breathing tube inserted through the trachea) to administer oxygen.
Your veterinarian will also likely place an intravenous (IV) catheter in your dog. This catheter allows IV fluids to be administered in order to keep the lungs moist and decrease the risk of complications. Additionally, your dog may be unwilling or unable to drink water for the first few days after smoke inhalation, so IV fluids can be used to prevent dehydration.
Smoke inhalation often results in painful burns, so your veterinarian will also administer pain medication to your dog. Affected dogs are typically given injectable pain medications to keep them comfortable. Oral anesthetic rinses may also be used, if burns within the mouth are present.
“Smoke inhalation often results in painful burns, so your veterinarian will also administer pain medication to your dog.”
Your dog may also receive bronchodilators to help keep his airways open, if needed. In some cases, antibiotics may be required to treat secondary infections that can occur following lung damage.
In some cases, dogs may require additional supportive care, such as nebulization and coupage. These techniques can be used to deliver medication directly to the lungs and to remove lung secretions. See the handout “Techniques for Nebulization and Coupage in Dogs” for more information on these techniques.
What is the prognosis with smoke inhalation?
Most dogs with smoke inhalation have a good prognosis. Estimated survival rates for animals without skin burns are approximately 90%, according to multiple studies.
Dogs that present with neurologic signs, extensive skin burns, or whose condition deteriorates on the second day of hospitalization typically experience worse outcomes. The prognosis is guarded for these patients.
Contributors: Catherine Barnette, DVM
© Copyright 2019 LifeLearn Inc. Used and/or modified with permission under license.
Cranial Cruciate Ligament Repair: Tibial Plateau Leveling Osteotomy (TPLO)
One of the most common injuries to the knee of dogs is tearing of the cranial cruciate ligament (CCL). This ligament is similar to the anterior cruciate ligament (ACL) in humans. There are actually two cruciate ligaments inside the knee: the cranial cruciate ligament and caudal cruciate ligament. They are called cruciate because they cross over each other inside the middle of the knee.
When the CCL is torn or injured, the shin bone (tibia) shin bone slides forward with respect to the thigh bone (femur), which is known as a positive drawer sign. Most dogs with this injury cannot walk normally and experience pain. The resulting instability damages the cartilage and surrounding bones and leads to osteoarthritis (OA).
What options are there for repairing my dog’s torn CCL?
When the cranial cruciate ligament is torn, surgical stabilization of the knee joint is often required, especially in larger or more active dogs. Surgery is generally recommended as quickly as possible to reduce permanent, irreversible joint damage and relieve pain.
“Surgery is generally recommended
as quickly as possible to reduce
permanent, irreversible joint damage
and relieve pain.”
Several surgical techniques are currently used to correct CCL rupture. Each procedure has unique advantages and potential drawbacks. Your veterinarian will guide you through the decision-making process and advise you on the best surgical option for your pet.
My veterinarian is recommending a tibial plateau leveling osteotomy to fix my dog’s torn CCL. What does this surgery involve?
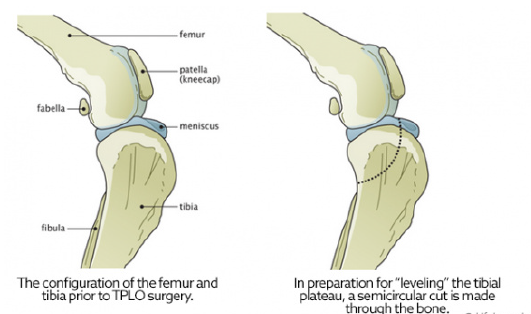
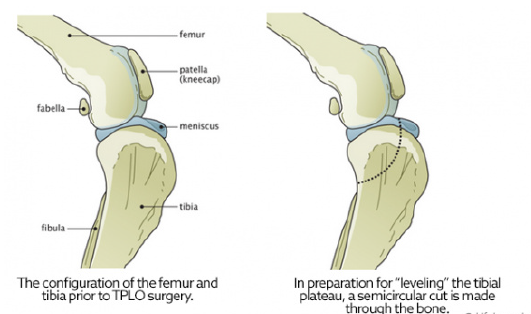
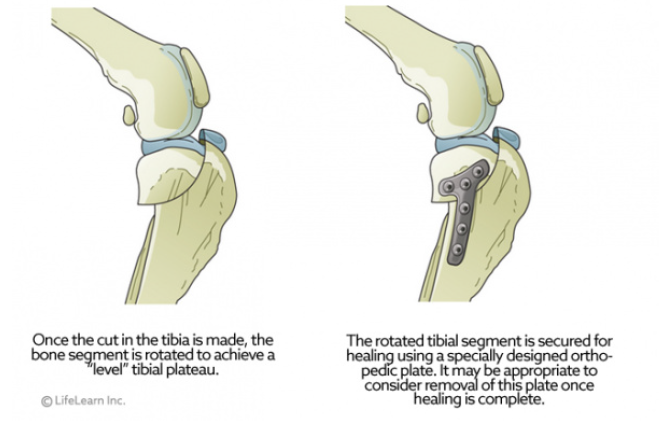
A major advancement in the treatment of CCL rupture has been the development of tibial plateau leveling osteotomy or TPLO. This surgery changes the angle and relationship of the femur and the tibia. The overall intent of the surgery is to reduce the amount that the tibia shifts forward during a stride. This is accomplished by making a semicircular cut through the top of the tibia, rotating the top of the tibia, and using a bone plate to allow the tibia to heal. This realignment of the surfaces within the stifle (knee) helps to provide stability during a stride and helps to reduce future joint inflammation and OA. By carefully adjusting the angle or slope of the top of the tibia, surgeons are able to replicate a more normal configuration of the knee joint and reduce mechanical stress.
“A major advancement in the treatment of CCL injuries has been the development of TPLO.”
To better understand the purpose of leveling the tibia, we often use the analogy of a wagon on a hill. Imagine a wagon tied to a post on the slope of a hill. As long as the rope holds, the wagon does not roll downhill. If we add excess weight (or downward force) to the wagon, the rope could break, and the wagon will roll down the hill. However, if the wagon is on level ground, it will not roll forward with added weight, even if the rope is broken.
In this example, the wagon is the femur, and it slides down slope of the top of the tibia when the CCL is ruptured. This instability leads to damage and destruction of the cartilage and bones of the knee joint. TPLO surgery levels the tibia to prevent the femur from sliding forward, thereby stabilizing the
joint.
TPLO surgery involves making a curved cut in the tibia from the front to the back, much like half a smiley face. The top section of the tibia is then rotated backward until the angle between the tibia and femur is deemed
appropriately level, typically between 2 and 14 degrees, with 5 degrees being the ideal angle. A metal bone plate is then used to affix the two sections of tibia in the desired positions, allowing the tibia to heal in its new configuration.
How long will it take for my dog to recover from TPLO surgery?
Healing from TPLO surgery is generally rapid.
- About half of all canine patients will begin walking on the injured leg within 24 hours after surgery.
- At 2 weeks postoperatively, most dogs are bearing moderate to complete amounts of weight on the affected leg.
- By 10 weeks, most dogs do not have an appreciable limp or gait abnormality.
- As mentioned above, at 4 months postoperatively, the majority of dogs can begin walking and playing normally, with only the stressful activities restricted.
- Within 6 months, most dogs can resume full physical activity.
Pain management during and after stifle (knee) surgery is critical, so be sure to give all medications as prescribed and use them until they are gone. Physical rehabilitation post-operatively will speed healing. Ask your veterinarian about incorporating rehabilitation into your dog’s recovery plan.
“Pain management during and after stifle (knee) surgery is critical, so be sure to give all medications as prescribed and use them until they are gone.”
The most common complication after TPLO is infection. Studies conclude that infection occurs in less than 10% of all patients, with many surgeons reporting much lower complication rates. Your dog will need several recheck examinations and radiographs (X-rays) to ensure that the area is healing properly.
Contributors: Tammy Hunter, DVM; Robin Downing, DVM, DAAPM, DACVSMR, CVPP, CRPP
© Copyright 2019 LifeLearn Inc. Used and/or modified with permission under license.
Ringworm in Dogs
Ringworm” is the common name given to a fungal infection of the superficial layers of the skin, hair and nails. Ringworm infections can occur in humans and in all domesticated species of animals. The common name of ringworm is somewhat misleading, in that it is not an infection caused by a worm, and the infected areas are not always ring-shaped. The fungi responsible for ringworm infections belong to a specialized group known as dermatophytes, so the medical name for this disease is dermatophytosis. Read on for more about Ringworm…
Sebaceous Adenitis
Sebaceous adenitis is an immune-mediated disorder in which there is an inflammatory process directed against the sebaceous glands in the skin. There are two forms of the disease, one that occurs in short-haired breeds and one that occurs in long-haired breeds. Read on to see how the disorder differs by breed and for available treatment options.