Spontaneous Pneumothorax
Spontaneous pneumothorax can be seen in both dogs and cats and occurs with no history of trauma or iatrogenic penetration into the thoracic cavity. The normal physiologic negative pressure within the thorax that maintains inflation of the lungs is lost, air will accumulate within the thorax and the lungs will collapse. There are two access routes allowing air into the thorax that will result in a spontaneous pneumothorax: the airways and the esophagus. The first occurs when there is compromise of lung or tracheal tissue resulting in air escaping into the thoracic cavity. Compromised lung tissue leading to a spontaneous pneumothorax is often caused by bullae or bleb formation at the edges of the lung lobes. These are tiny air-filled sacs that can rupture within the thorax (Figure 1). Bullae and blebs are most frequently found in dogs with no concurrent lung disease and it is the most common cause of spontaneous pneumothorax. Bullae and blebs are less common in cats, but they are the main cause of feline cases of spontaneous pneumothorax.
The second route of entry into the thorax is from esophageal perforation that results in both pneumothorax and additional air accumulation in secondary locations causing subcutaneous emphysema or pneumomediastinum. Secondary causes of spontaneous pneumothorax in dogs include cancer, bacterial pneumonia, fungal infection, pulmonary abscesses, grass awn migration, pulmonary thromboembolism, and heartworm disease. In cats, spontaneous pneumothorax can be caused by inflammatory airway disease, heartworm or lungworm infection, and bronchopulmonary dysplasia. In some patients the cause is unknown.
Spontaneous pneumothorax occurs primarily in deep-chested, large breed dogs with no sex predilection. Siberian Huskies and other Northern breeds are overrepresented. There are no known common associations in cats. Clinical signs noted in dogs include increased respiratory rate, cough, anxiety, cyanosis, overinflation of the thorax, and an orthopneic posture. Common signs noted in cats are respiratory distress, cough, collapse, lethargy, anorexia, and vomiting.
Initially, we recommend 3-view thoracic radiographs to assess for pneumothorax (Figure 2). This diagnostic test rarely confirms the underlying cause and additional advanced imaging such as a CT scan often becomes necessary (Figure 3). Before referral, a therapeutic thoracocentesis along the dorsolateral thorax is necessary to stabilize the patient, as well as supplemental oxygen therapy. Once the patient arrives at our facility, we will reassess with thoracic radiographs or TFAST for an additional accumulation of air. Before the CT scan, we will do an additional thoracocentesis or place chest tubes to keep air out of the cavity and allow the lungs to fully expand for imaging. Supplemental oxygen will be necessary at all times to assist with increased oxygen delivery to the body.
Treatment options vary depending on the severity of the clinical signs. The underlying cause of spontaneous pneumothorax dictates which treatment option will be most appropriate. Most often, spontaneous pneumothorax cannot be managed medically (oxygen supplementation and chest tube management) long-term, and surgical intervention is warranted to remove the primary cause of the pneumothorax.
Surgical treatment most often includes a lung lobectomy. This can be accomplished using three different approaches to the thorax: minimally invasive thoracoscopy, median sternotomy, or lateral thoracotomy. The choice of the approach depends on the underlying cause of the disease and the location of the affected lung lobe. If laterality is determined via the CT scan then a thoracotomy is the best option. If we cannot determine the cause then a median sternotomy is chosen. Once the thoracic cavity is open, each lung lobe is inspected for an abnormality causing a leak. If no overt abnormality is noted, the thoracic cavity is filled with warm saline; bubbles will appear in the saline from the lung lobe that is affected. Stapling equipment is used to remove the lung lobe at the base. The lobe will be submitted for histopathology. The warm saline will be used again to assess the remaining bronchus for any leaks. If a chest tube was not placed before surgery, one is placed before closing the thorax.
We will monitor chest tube production in the ICU postoperatively. Once air and fluid are no longer accumulating (and being removed via the tube), the tube is removed and the patient will most likely be discharged the next day.
Long-term outcomes for dogs with spontaneous pneumothorax are excellent with surgical intervention and lung lobectomy. Very rarely are cases not amenable to surgical resection and those patients’ prognoses vary depending on the severity of the disease. Recurrence rates of spontaneous pneumothorax are approximately 3% with surgical treatment and as high as 50% with medical treatment. Mortality rates reflect the need for appropriate surgical management. The mortality rate with surgery is 12% and is over 50% with medical management.
Outcome data for cats is more limited. The prognosis can still be good overall depending on the underlying cause and response to therapy. In a previous study, 54% of the cats evaluated survived to discharge with the majority being treated medically. For cats with small volume pneumothoraces, conservative therapy with oxygen and chest tube /thoracocentesis may offer a good outcome. Surgery may be needed in severe cases or when there is persistent pneumothorax present despite medical management.
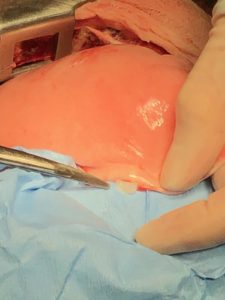
Figure 1 – A bleb is noted along the periphery of the lung lobe.

Figure 2 – Left lateral radiograph of a dog with a pneumothorax. Note the collapse of the lung lobe (thin arrow) and the raised heart.
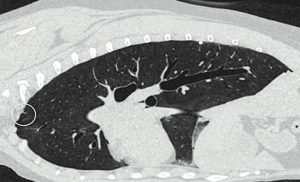
Figure 3 – A sagittal view of a CT scan of a dog with a bleb on the periphery of the lung lobe (circle).
Article Written By:
Catherine Loughin, DVM
DACVS, DACCT
Soft Tissue, Oncologic, Orthopedic, Neurosurgery


