Category: Surgery
Cranial Cruciate Ligament Repair: Tibial Plateau Leveling Osteotomy (TPLO)
One of the most common injuries to the knee of dogs is tearing of the cranial cruciate ligament (CCL). This ligament is similar to the anterior cruciate ligament (ACL) in humans. There are actually two cruciate ligaments inside the knee: the cranial cruciate ligament and caudal cruciate ligament. They are called cruciate because they cross over each other inside the middle of the knee.
When the CCL is torn or injured, the shin bone (tibia) shin bone slides forward with respect to the thigh bone (femur), which is known as a positive drawer sign. Most dogs with this injury cannot walk normally and experience pain. The resulting instability damages the cartilage and surrounding bones and leads to osteoarthritis (OA).
What options are there for repairing my dog’s torn CCL?
When the cranial cruciate ligament is torn, surgical stabilization of the knee joint is often required, especially in larger or more active dogs. Surgery is generally recommended as quickly as possible to reduce permanent, irreversible joint damage and relieve pain.
“Surgery is generally recommended
as quickly as possible to reduce
permanent, irreversible joint damage
and relieve pain.”
Several surgical techniques are currently used to correct CCL rupture. Each procedure has unique advantages and potential drawbacks. Your veterinarian will guide you through the decision-making process and advise you on the best surgical option for your pet.
My veterinarian is recommending a tibial plateau leveling osteotomy to fix my dog’s torn CCL. What does this surgery involve?
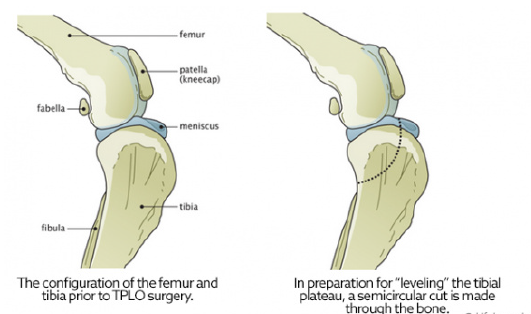
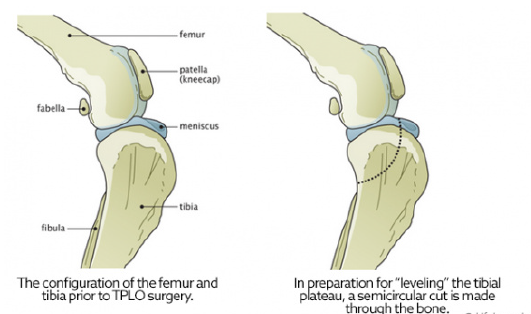
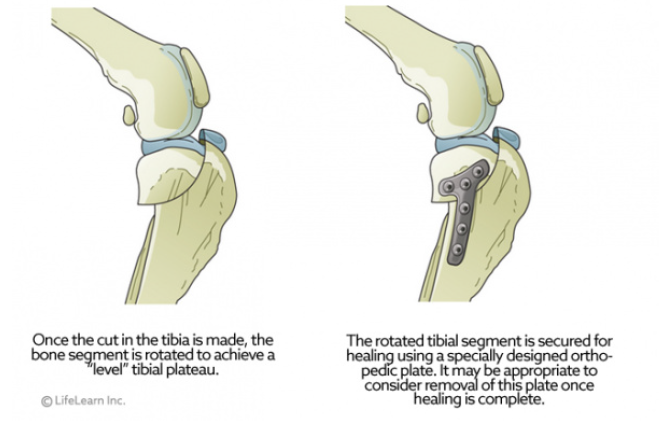
A major advancement in the treatment of CCL rupture has been the development of tibial plateau leveling osteotomy or TPLO. This surgery changes the angle and relationship of the femur and the tibia. The overall intent of the surgery is to reduce the amount that the tibia shifts forward during a stride. This is accomplished by making a semicircular cut through the top of the tibia, rotating the top of the tibia, and using a bone plate to allow the tibia to heal. This realignment of the surfaces within the stifle (knee) helps to provide stability during a stride and helps to reduce future joint inflammation and OA. By carefully adjusting the angle or slope of the top of the tibia, surgeons are able to replicate a more normal configuration of the knee joint and reduce mechanical stress.
“A major advancement in the treatment of CCL injuries has been the development of TPLO.”
To better understand the purpose of leveling the tibia, we often use the analogy of a wagon on a hill. Imagine a wagon tied to a post on the slope of a hill. As long as the rope holds, the wagon does not roll downhill. If we add excess weight (or downward force) to the wagon, the rope could break, and the wagon will roll down the hill. However, if the wagon is on level ground, it will not roll forward with added weight, even if the rope is broken.
In this example, the wagon is the femur, and it slides down slope of the top of the tibia when the CCL is ruptured. This instability leads to damage and destruction of the cartilage and bones of the knee joint. TPLO surgery levels the tibia to prevent the femur from sliding forward, thereby stabilizing the
joint.
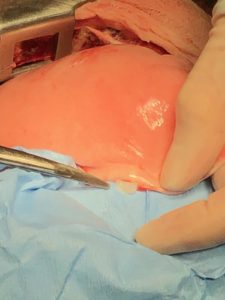
TPLO surgery involves making a curved cut in the tibia from the front to the back, much like half a smiley face. The top section of the tibia is then rotated backward until the angle between the tibia and femur is deemed
appropriately level, typically between 2 and 14 degrees, with 5 degrees being the ideal angle. A metal bone plate is then used to affix the two sections of tibia in the desired positions, allowing the tibia to heal in its new configuration.
How long will it take for my dog to recover from TPLO surgery?
Healing from TPLO surgery is generally rapid.
- About half of all canine patients will begin walking on the injured leg within 24 hours after surgery.
- At 2 weeks postoperatively, most dogs are bearing moderate to complete amounts of weight on the affected leg.
- By 10 weeks, most dogs do not have an appreciable limp or gait abnormality.
- As mentioned above, at 4 months postoperatively, the majority of dogs can begin walking and playing normally, with only the stressful activities restricted.
- Within 6 months, most dogs can resume full physical activity.
Pain management during and after stifle (knee) surgery is critical, so be sure to give all medications as prescribed and use them until they are gone. Physical rehabilitation post-operatively will speed healing. Ask your veterinarian about incorporating rehabilitation into your dog’s recovery plan.
“Pain management during and after stifle (knee) surgery is critical, so be sure to give all medications as prescribed and use them until they are gone.”
The most common complication after TPLO is infection. Studies conclude that infection occurs in less than 10% of all patients, with many surgeons reporting much lower complication rates. Your dog will need several recheck examinations and radiographs (X-rays) to ensure that the area is healing properly.
Contributors: Tammy Hunter, DVM; Robin Downing, DVM, DAAPM, DACVSMR, CVPP, CRPP
© Copyright 2019 LifeLearn Inc. Used and/or modified with permission under license.